Meningococcemia
Meningococcal septicemia; Meningococcal blood poisoning; Meningococcal bacteremiaMeningococcemia is an acute and potentially life-threatening infection of the bloodstream.
Acute
Acute means sudden. Acute symptoms appear, change, or worsen rapidly. It is the opposite of chronic.

Causes
Meningococcemia is caused by bacteria called Neisseria meningitidis. The bacteria often live in a person's upper respiratory tract without causing signs of illness. They can be spread from person to person through respiratory droplets. For example, you may become infected if you are around someone with the condition and they sneeze or cough.
Family members and those closely exposed to someone with the condition are at increased risk. The infection occurs more often in winter and early spring.
Symptoms
Some of the initial symptoms include:
- Fever
- Headache
- Irritability
- Muscle pain
- Nausea
- Rash with very small red or purple spots on the feet or legs
Later symptoms may include:
- A decline in your level of consciousness
Decline in your level of consciousness
Decreased alertness is a state of reduced awareness and is often a serious condition. A coma is the most severe state of decreased alertness in which...
Read Article Now Book Mark Article - Large areas of bleeding under the skin
- Shock
Shock
Shock is a life-threatening condition that occurs when the body is not getting enough blood flow. Lack of blood flow means the cells and organs do n...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Exams and Tests
Your health care provider will examine you and ask about your symptoms.
Blood tests will be done to check for other infections and help confirm meningococcemia. Such tests may include:
- Blood culture
Blood culture
A blood culture is a laboratory test to check for bacteria or other germs in a blood sample.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Complete blood count with white cell differential
Complete blood count
A complete blood count (CBC) test measures the following:The number of white blood cells (WBC count)The number of red blood cells (RBC count)The numb...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Blood clotting studies
Other tests that may be done include:
- Lumbar puncture to get a sample of cerebrospinal fluid for Gram stain and culture
Lumbar puncture
Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. CSF acts as a cushion, protecting the b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleGram stain
A Gram stain is a test used to identify bacteria. It is one of the most common ways to quickly diagnose bacterial infection in the body.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleCulture
A cerebrospinal fluid (CSF) culture is a lab test to look for bacteria, fungi, and viruses in the fluid that moves in the space around the spinal cor...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Skin biopsy and Gram stain and culture
Skin biopsy
A skin lesion biopsy is when a small amount of skin is removed so it can be examined under a microscope. The skin is tested to look for skin conditi...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urine analysis
Urine analysis
Urinalysis is the physical, chemical, and microscopic examination of urine. It involves a number of tests to detect and measure various compounds th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
Treatment
Meningococcemia is a medical emergency. People with this infection are often admitted to the intensive care unit of the hospital, where they are closely monitored. They may be placed in respiratory isolation for the first 24 hours to help prevent the spread of the infection to others.
Treatments may include:
- Antibiotics given through a vein immediately
- Breathing support
- Clotting factors or platelet replacement, if bleeding disorders develop
Bleeding disorders
Bleeding disorders are a group of conditions in which there is a problem with the body's blood clotting process. These disorders can lead to heavy a...
Read Article Now Book Mark Article - Fluids through a vein
- Medicines to treat low blood pressure
- Wound care for areas of skin with blood clots
Outlook (Prognosis)
Early treatment results in a good outcome. When shock develops, the outcome is less certain.
The condition is most life threatening in those who develop:
- A severe bleeding disorder called disseminated intravascular coagulopathy (DIC)
Disseminated intravascular coagulopathy...
Disseminated intravascular coagulation (DIC) is a serious disorder in which the proteins that control blood clotting become overactive.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Kidney failure
- Shock
Possible Complications
Possible complications of this infection are:
- Arthritis
Arthritis
Arthritis is inflammation or degeneration of one or more joints. A joint is the area where 2 bones meet. There are more than 100 different types of...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Bleeding disorder (DIC)
- Gangrene due to lack of blood supply
- Inflammation of blood vessels in the skin
- Inflammation of the heart muscle
- Inflammation of the heart lining
- Shock
- Severe damage to the adrenal glands that can lead to low blood pressure (Waterhouse-Friderichsen syndrome)
Waterhouse-Friderichsen syndrome
Waterhouse-Friderichsen syndrome (WFS) is a group of symptoms caused when the adrenal glands fail to function normally. This occurs as a result of b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
When to Contact a Medical Professional
Go to the emergency room immediately if you have symptoms of meningococcemia. Contact your provider if you have been around someone with the disease.
Prevention
Preventive antibiotics for family members and other close contacts are often recommended. Contact your provider about this option.
A vaccine that covers some, but not all, strains of meningococcus is recommended for children age 11 or 12. A booster is given at age 16. Unvaccinated college students who live in dormitories should also consider receiving this vaccine. It should be given a few weeks before they first move into the dorm. Talk to your provider about this vaccine.
Vaccine
All content below is taken in its entirety from the CDC Meningococcal ACWY Vaccine Information Statement (VIS): www. cdc. gov/vaccines/hcp/current-vi...

References
Marquez L. Meningococcal disease. In: Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, eds. Feigin and Cherry's Textbook of Pediatric Infectious Diseases. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 88.
Stephens DS, Apicella MA. Neisseria meningitidis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 211.
Stephens DS. Neisseria meningitidis infections. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 274.
Bacteria - illustration
Bacterial infections can lead to the formation of pus, or to the spread of the bacteria in the blood.
Bacteria
illustration
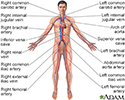
Circulatory system - illustration
Blood used by the body is brought back to the heart and lungs by the veins of the body. Once the blood has gathered more oxygen from the lungs, it is pumped back out to the body through the arteries.
Circulatory system
illustration
Upper respiratory tract - illustration
The major passages and structures of the upper respiratory tract include the nose or nostrils, nasal cavity, mouth, throat (pharynx), and voice box (larynx). The respiratory system is lined with a mucous membrane that secretes mucus. The mucus traps smaller particles like pollen or smoke. Hairlike structures called cilia line the mucous membrane and move the particles trapped in the mucus out of the nose. Inhaled air is moistened, warmed, and cleansed by the tissue that lines the nasal cavity.
Upper respiratory tract
illustration
Bacteria - illustration
Bacterial infections can lead to the formation of pus, or to the spread of the bacteria in the blood.
Bacteria
illustration
Circulatory system - illustration
Blood used by the body is brought back to the heart and lungs by the veins of the body. Once the blood has gathered more oxygen from the lungs, it is pumped back out to the body through the arteries.
Circulatory system
illustration
Upper respiratory tract - illustration
The major passages and structures of the upper respiratory tract include the nose or nostrils, nasal cavity, mouth, throat (pharynx), and voice box (larynx). The respiratory system is lined with a mucous membrane that secretes mucus. The mucus traps smaller particles like pollen or smoke. Hairlike structures called cilia line the mucous membrane and move the particles trapped in the mucus out of the nose. Inhaled air is moistened, warmed, and cleansed by the tissue that lines the nasal cavity.
Upper respiratory tract
illustration
Review Date: 11/10/2024
Reviewed By: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.